Revolutionizing Severe Periodontal Care: Transformative Results with PerioDT® Biofilm Debridement
Industry
Periodontal Care
Challenge
Patient with generalized severe gingival inflammation and bleeding, heavy plaque and calculus accumulation, and multiple sites exhibiting probing depths of 8mm.
Results
A significant reduction in bleeding on probing, and the probing depths had improved considerably, with many sites reducing by 2mm or more in just 3 weeks.
Product Used
PerioDT
"The patient was visibly pleased and reported feeling 'so much better,' noting a significant reduction in gum pain and no longer experiencing spontaneous bleeding during brushing or eating."

Anna Hancock
Registered Dental Hygienist

Patient History
The patient, a middle-aged male, presented to our office with the chief complaint: “My gums bleed and hurt sometimes.” Upon initial examination, it was evident that the patient had not received a professional dental cleaning in many years.
Clinical signs included generalized severe gingival inflammation, heavy plaque and calculus accumulation, and multiple sites exhibiting probing depths of 8mm. Bleeding on probing (BOP) was widespread. Based on the clinical findings and patient history, he was diagnosed with generalized stage III, grade B periodontitis.

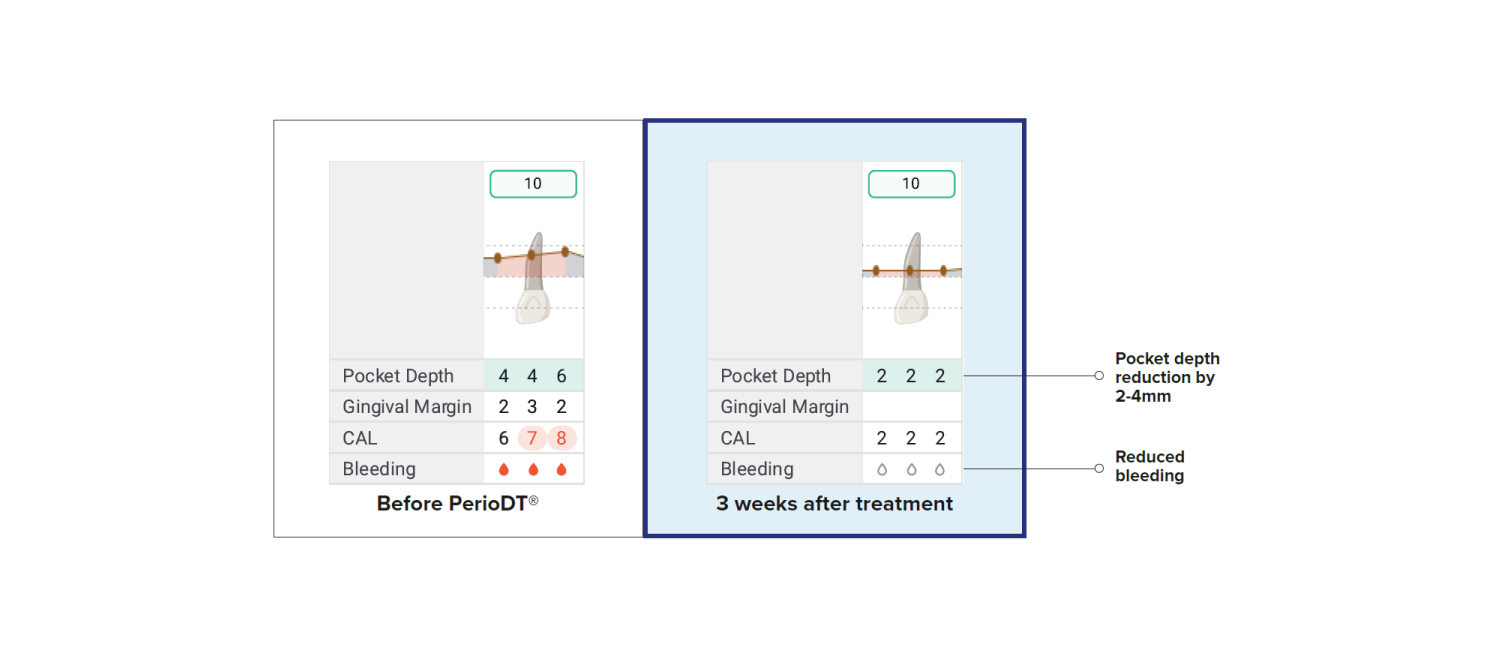
Probing Depths & Bleeding Before TreatmentcBefore treatment images taken April 1, 2025. After treatment images taken April 24, 2025.
 Incorporation of PerioDT
Incorporation of PerioDT
Given the severity of the inflammation and the impressive outcomes we have consistently achieved with PerioDT in our periodontal therapy cases, I made the decision to incorporate it into his non-surgical periodontal treatment plan.
From prior clinical experiences, I’ve seen PerioDT significantly enhance healing and reduce inflammation more rapidly compared to traditional SRP alone. I was confident the patient would benefit tremendously from its inclusion.
"The patient was scheduled for an initial follow-up appointment 3 weeks post-treatment. At this visit, the improvements were remarkable."
Application Technique
Before any other treatment—topical anesthetic or local anesthetic—I applied PerioDT to maximize its absorption and therapeutic impact. The treatment site was dried thoroughly to ensure optimal adhesion and retention of the gel.
Application began by placing the PerioDT directly under the gingival margin in the affected areas. In interproximal sites, the tip of the delivery syringe was carefully inserted to the base of each pocket, allowing the gel to fill the entire depth. Buccal and lingual areas were treated in a similar fashion to ensure comprehensive coverage.
After placement, I allowed the PerioDT to remain undisturbed for 10–30 seconds before gently rinsing the area with water. This was followed by thorough scaling and root planing of all affected areas.
Follow-Up Timeline and Outcomes
The patient was scheduled for an initial follow-up appointment 3 weeks post-treatment. At this visit, the improvements were remarkable. There was a significant reduction in bleeding on probing, and the probing depths had improved considerably, with many sites reducing by 2mm or more in just 3 weeks.

Before treatment image taken April 1, 2025. After treatment image taken April 24, 2025.
The gingival tissues appeared much healthier, with decreased erythema and edema. The patient was visibly pleased and reported feeling “so much better,” noting a significant reduction in gum pain and no longer experiencing spontaneous bleeding during brushing or eating.
Future maintenance visits are planned to continue monitoring healing and reinforce home care. The patient is now highly motivated and has committed to maintaining regular periodontal maintenance appointments.
Conclusion
This case exemplifies how the integration of PerioDT into the periodontal therapy workflow can dramatically enhance treatment outcomes, especially in severe cases.
By prioritizing its application at the beginning of treatment and utilizing a careful, methodical placement technique, we were able to promote rapid healing and significantly improve clinical parameters in a short time frame.
After Treatment
Probing Depths & Bleeding After Treatment

